*This information was originally published as part of an abstract for ATS 2O25*
Understanding COPD and the Unmet Patient Need
Many people living with chronic obstructive pulmonary disease (COPD) experience frequent flare-ups that make it harder to breathe, lead to repeated hospital visits, and reduce their overall quality of life. Despite available treatments, symptoms often remain poorly controlled, especially for those in the exacerbation-prone group (E Group).
Recent FDA approval of a biologic therapy that targets the interleukin-4 and interleukin-13 pathways, key drivers of type 2 (T2) inflammation, represents a meaningful advancement. Further education is needed to support awareness and adoption of updated best practices for treating patients who are most vulnerable to exacerbations.
The Medlive Approach
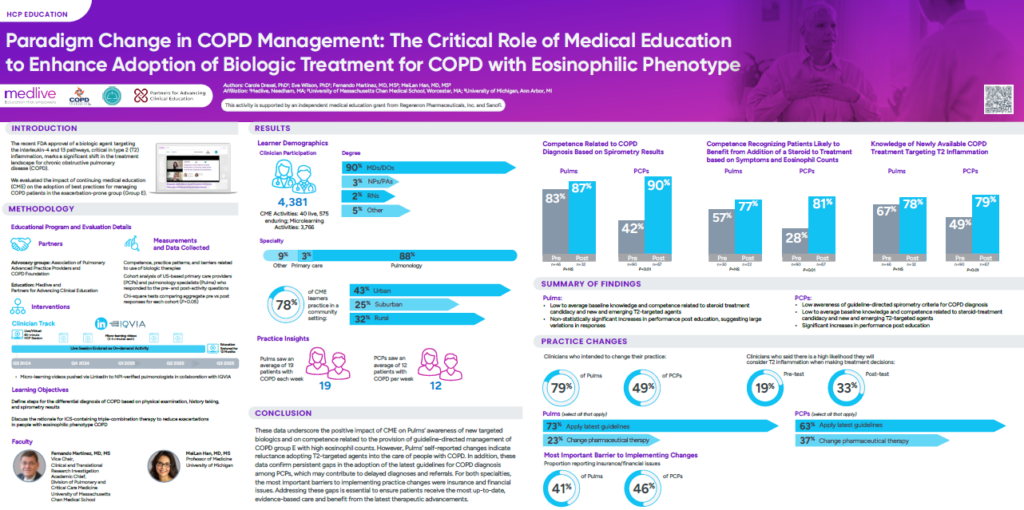
At Medlive, we believe that we can help overcome these barriers through targeted digital education. To that end, we joined forces with the Association of Pulmonary Advanced Practice Providers (APAPP) and the COPD Foundation to deliver an educational initiative titled “Diagnosis and Evidence-based Prevention of Chronic Obstructive Pulmonary Disease Exacerbations.” This included a clinician track for NPI-verified pulmonologists (1-hour online CME activity broadcast live and available on-demand for a year and microlearning videos pulsed through social media) and a patient/caregiver track (patient vignettes pulsed through social media).
The outcomes poster for this program was presented by Medlive Medical Director Carole Drexel at the ATS 2025 International Conference.
Data Analysis
Over 4,300 clinicians participated in the COPD education, with 59% of them in primary care and pulmonology specialties. The key takeaways from the program data were:
- Significant Knowledge Gains: Clinicians demonstrated substantial improvements across core learning objectives. PCPs improved in recognizing spirometry thresholds for COPD diagnosis (42% to 90%, p<0.01) and in identifying patients appropriate for inhaled steroid treatment based on symptoms and eosinophil counts (28% to 81%, p<0.01). Pulmonologists also showed gains in recognizing steroid candidacy (57% to 77%, p<0.01) and in identifying the mechanism of dupilumab (67% to 78%, p<0.01).
- Intent to Implement Change: 79% of pulmonology learners and 49% of PCPs reported intent to change clinical practice. Planned changes focused primarily on applying updated COPD guidelines and secondarily on changing pharmaceutical therapies for both Pulmonology and PCP learners.
Together, these findings reinforce the critical role of targeted education in closing knowledge gaps and supporting the adoption of evidence-based care.
Conclusion – Collaborating for Improved Patient Outcomes
If you’d like to learn more about working with Medlive, fill out the form on our contact us page to get-in-touch.