*This information was originally published as part of an abstract for the 2025 ASCO Quality Care Symposium.*
Understanding NSCLC and the Unmet Patient Need
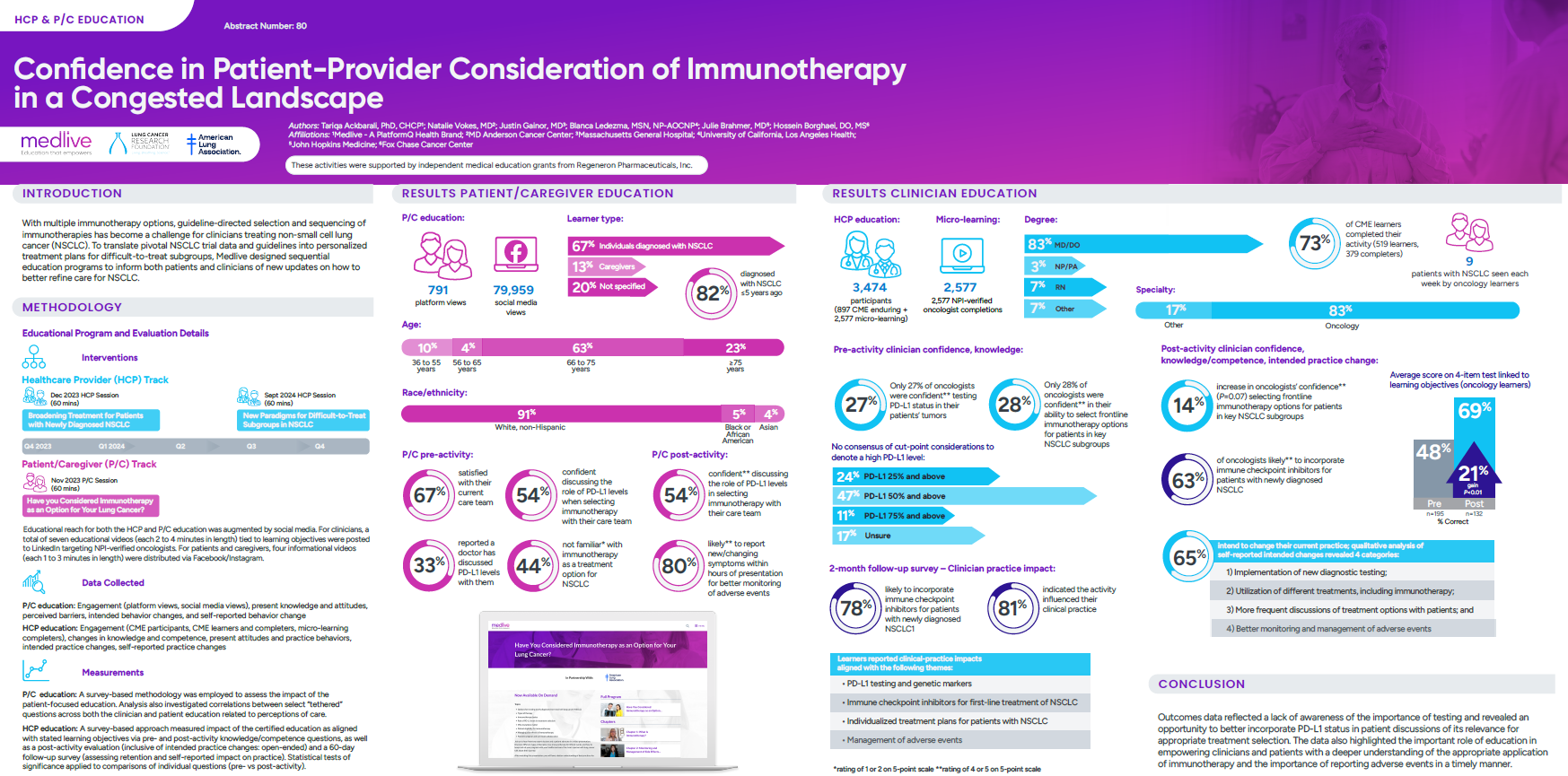
The treatment of non-small cell lung cancer (NSCLC) is becoming increasingly complex, as the availability of multiple immunotherapy options has made guideline-directed selection and sequencing a significant challenge, particularly for difficult-to-treat subgroups.
As oncology teams and caregivers work to integrate these therapies, there is a clear need to strengthen awareness, acceptance, and readiness so that healthcare providers (HCPs) have the guidance necessary to apply new strategies with confidence, and patients and caregivers (P/Cs) are prepared to engage in informed treatment discussions.
The Medlive Approach
To address gaps in knowledge and support both clinical decision-making and patient engagement in NSCLC, Medlive launched a series of targeted digital education programs.
To support translation of pivotal trial data and evolving guidelines into personalized treatment plans, Medlive joined forces with the American Lung Association and the Lung Cancer Research Foundation to develop sequential education programs aimed at equipping both clinicians and patients with the latest updates.
“Quality care in lung cancer isn’t just about treatment—it’s about ensuring patients and care teams have the information they need to make confident decisions. Working with Medlive gives us one more way to share knowledge in a practical, accessible way that can make a real difference in the clinic and in people’s lives.”
– Courtney Brandt, Director, Educational Programs, Lung Cancer Research Foundation (LCRF)
The first initiative, hosted in November 2023, delivered a 60-minute CME activity for medical and thoracic oncologists, pathologists, oncology nurse practitioners, and physician assistants, offered as a live virtual event and subsequently available online for one year.
This was complemented by patient-focused education designed for individuals with NSCLC and their caregivers, which was also offered as a 60-minute live virtual program and later adapted into two enduring online chapters.
A follow-up clinician education activity was held in September 2024, consisting of an on-demand, three-module CME series (60 minutes total) that reinforced best practices for patient selection in difficult-to-treat subgroups.
Collectively, these initiatives reflect Medlive’s tethered educational design, ensuring that both HCPs and P/Cs had access to timely, evidence-based guidance to inform the integration of immunotherapy into NSCLC care.
Key Findings
- P/C Impact: Strong engagement was achieved with nearly 80,000 social media views and 750+ platform views. Before education, less than half were familiar with immunotherapy, and only one-third reported PD-L1 discussions with their physician. Post-activity, 80% indicated they were more likely to report new or changing symptoms within hours of presentation, demonstrating improved readiness to participate in care and better adverse event monitoring.
- HCP Impact: Education reached more than 3,400 oncology professionals, with 83% MD/DO participation and an average of nine NSCLC patients seen per week. Confidence in selecting frontline immunotherapy improved by 14%, and nearly two-thirds intended to change practice—most commonly by expanding diagnostic testing, refining treatment selection, enhancing patient discussions, and strengthening adverse event (AE) management. At the 2-month follow-up survey, 78% were likely to incorporate immune checkpoint inhibitors in newly diagnosed NSCLC, and 81% reported that the activity had influenced their clinical practice, underscoring sustained impact on care delivery.
Conclusion – Collaborating for Improved Patient Outcomes
The outcomes data reflected limited awareness of the importance of PD-L1 testing and underscored the need to more effectively integrate biomarker status into patient discussions to guide appropriate treatment selection. These results suggest a clear role for education in equipping both clinicians and patients with a deeper understanding of immunotherapy application in NSCLC and the importance of timely reporting of adverse events. Taken together, the findings highlight the essential role of education in closing knowledge gaps, overcoming adoption challenges, and empowering shared decision-making. By improving awareness and confidence in the use of PD-L1 testing and immune checkpoint inhibitors, care teams can better tailor treatment strategies to patient needs and ultimately improve outcomes.
To learn more about partnering with Medlive to develop impactful CME programs, reach out via our Contact Us page.
This initiative was supported by an independent educational grant from Regeneron Pharmaceuticals, Inc.




